Hard skills , such as skills in data management systems, knowledge of healthcare regulations, and expertise in patient enrollment processes, are essential for effective job performance.
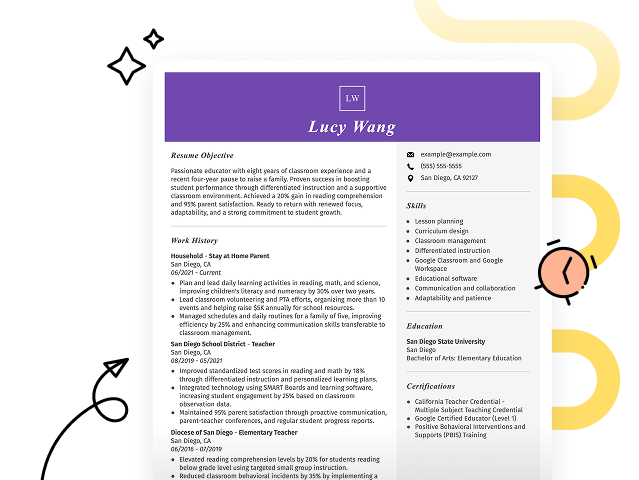
Popular Enrollment Specialist Resume Examples
Check out our top enrollment specialist resume examples that emphasize skills like customer service, data management, and effective communication. These examples demonstrate how to showcase your qualifications in a way that captivates hiring managers.
Ready to build your ideal resume? Our Resume Builder offers user-friendly templates specifically designed for professionals in enrollment and admissions, helping you make a great impression.
Recommended
Entry-level enrollment specialist resume
This entry-level resume effectively highlights the applicant's ability to manage and optimize enrollment processes, showcasing their expertise in CRM systems and strategic communication. New professionals in this field should demonstrate their ability to improve processes and engage students effectively, even with limited direct experience.
Mid-career enrollment specialist resume
This resume effectively emphasizes key qualifications, showcasing the applicant's accomplishments and impact in enrollment management. The progression from student services to leadership roles highlights readiness for advanced responsibilities, illustrating a strong commitment to improving processes and improving student experiences.
Experienced enrollment specialist resume
This resume's work history section reflects the applicant's strong expertise in enrollment management, demonstrating their success in increasing enrollment by 15% and improving application processing times by 20%. The clear bullet-point format improves readability, making it easy for hiring managers to quickly grasp key achievements.
Resume Template—Easy to Copy & Paste
Daniel Davis
Chicago, IL 60611
(555)555-5555
Daniel.Davis@example.com
Professional Summary
Dynamic Enrollment Specialist with 4 years in boosting enrollments using strategic CRM and recruitment methods. Proven track record in enhancing process efficiency and lead generation.
Work History
Enrollment Specialist
Strategic Education Partners - Chicago, IL
June 2024 - October 2025
- Boosted enrollment by 15% within one year.
- Developed outreach plan increasing leads by 20%.
- Reduced enrollment processing time by 30%.
Student Admissions Coordinator
Future Scholars Academy - Springfield, IL
January 2022 - May 2024
- Managed applicant pool, enhancing selection process.
- Implemented CRM system, improving efficiency by 25%.
- Engaged with 50 schools to source diverse candidates.
Academic Enrollment Advisor
Western Education Consultants - Springfield, IL
January 2021 - January 2022
- Streamlined communication, reducing inquiry wait by 40%.
- Expanded programs, boosting enrollments by 10%.
- Organized 5 annual admission events.
Languages
- Spanish - Beginner (A1)
- French - Beginner (A1)
- Mandarin - Beginner (A1)
Skills
- Enrollment Management
- Student Recruitment
- CRM Software
- Strategic Planning
- Data Analysis
- Communication Skills
- Time Management
- Lead Generation
Certifications
- Certified Enrollment Management Professional - National Association for College Admission Counseling
- Advanced CRM Specialist - CRM Academy
Education
Master of Business Administration Business Management
Northeastern University Boston, Massachusetts
May 2020
Bachelor of Arts Education
University of California Los Angeles, California
May 2019
How to Write an Enrollment Specialist Resume Summary
Your resume summary is the first impression employers will have of you, making it important to convey your qualifications effectively. As an enrollment specialist, you should emphasize your expertise in managing student applications and guiding prospective students through the enrollment process.
Highlight your skills in communication, organization, and customer service, as these are vital for success in this role. You want to showcase how you can improve enrollment rates and improve the overall experience for applicants.
To gain a clearer picture of what makes an effective summary, consider the following examples that illustrate both successful and less effective approaches:
I am an enrollment specialist with many years of experience in the field. I am seeking a position where I can use my skills and make a positive impact on the organization. A job that offers flexibility and growth opportunities is what I desire. I believe I would be a great addition to your team if given the chance.
- Lacks specific examples of skills or achievements relevant to enrollment processes
- Emphasizes personal desires rather than showcasing how the job seeker can benefit the employer
- Contains generic phrases that do not highlight unique strengths or contributions
Results-driven enrollment specialist with over 4 years of experience in healthcare enrollment processes, excelling in patient outreach and data management. Successfully increased patient enrollment by 20% year-over-year through targeted marketing strategies and streamlined application procedures. Proficient in CRM software, compliance regulations, and cross-functional collaboration to improve service delivery.
- Begins with a clear statement of experience level and area of expertise
- Highlights a quantifiable achievement that showcases direct impact on enrollment numbers
- Mentions relevant technical skills and industry knowledge critical for the role of an enrollment specialist
Pro Tip
Showcasing Your Work Experience
The work experience section is important for your resume as an enrollment specialist, where you'll provide the bulk of your content. Effective resume templates always emphasize this key component.
This section should be organized in reverse-chronological order, detailing your past roles. Use bullet points to highlight specific achievements and contributions made in each position.
To help guide you, we'll share a couple of examples that illustrate what works well in showcasing your work history. These examples will clarify effective strategies and common pitfalls to avoid:
Enrollment Specialist
Future Education Solutions – Atlanta, GA
- Assisted students with enrollment
- Managed student records and data
- Communicated with prospective students
- Handled administrative tasks as needed
- Lacks specific employment dates
- Bullet points are overly generic and do not highlight achievements
- Focuses on basic responsibilities without demonstrating impact or results
Enrollment Specialist
ABC University – Los Angeles, CA
March 2020 - Present
- Manage the enrollment process for over 500 prospective students annually, ensuring compliance with institutional policies and deadlines
- Develop targeted outreach strategies that increased application submissions by 30% within one academic year
- Provide personalized support to students throughout the admissions journey, resulting in a 15% rise in student satisfaction scores
- Uses action verbs such as manage and develop to clearly convey the job seeker’s role and impact
- Incorporates specific metrics like percentages to highlight improvements and achievements
- Demonstrates relevant skills such as compliance knowledge and customer service skill through concrete examples
While your resume summary and work experience are important components, don’t overlook the importance of other sections. Each part plays a role in showcasing your qualifications. For more detailed guidance, visit our comprehensive guide on how to write a resume.
Top Skills to Include on Your Resume
A well-defined skills section is important for any resume as it allows you to immediately showcase your qualifications to potential employers. This part of the resume helps them quickly identify if you possess the essential capabilities needed for the enrollment specialist role.
For this position, you want your resume to showcase both hard skills and soft skills. Including a balanced mix of these two skills type assures employers you have the technical expertise and personal traits to succeed on the job.
Meanwhile, soft skills like strong communication, attention to detail, and problem-solving abilities play a important role in building rapport with patients and ensuring a smooth enrollment experience.
Selecting the right resume skills is important for aligning with employer expectations and passing automated screening systems. Many organizations use software to filter out applicants lacking key competencies for the position.
To effectively highlight your qualifications, review job postings carefully. These listings often provide valuable insights into which skills you should emphasize to catch the attention of recruiters and ensure your application meets ATS requirements.
Pro Tip
10 skills that appear on successful enrollment specialist resumes
Improve your resume to attract recruiters by incorporating essential skills that enrollment specialists need. Our resume examples highlight these skills, giving you the confidence to apply for positions with a professional touch.
Here are 10 key skills to consider including in your resume if they align with your qualifications and job demands:
Customer service expertise
Attention to detail
Effective communication
Data entry skills
Organizational abilities
Problem-solving skills
Familiarity with enrollment software
Multi-tasking capabilities
Time management
Team collaboration
Based on analysis of 5,000+ administrative professional resumes from 2023-2024
Resume Format Examples
Choosing the right resume format is important for enrollment specialists as it showcases their relevant skills, experience, and career growth in a clear and effective way.
Functional
Focuses on skills rather than previous jobs
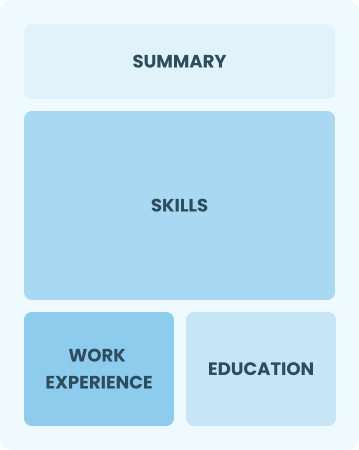
Best for:
Recent graduates and career changers with limited experience
Combination
Balances skills and work history equally
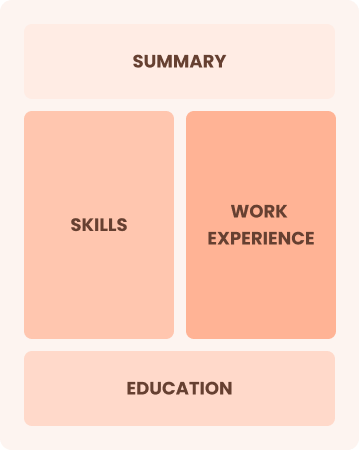
Best for:
Mid-career professionals focused on demonstrating their skills and growth potential
Chronological
Emphasizes work history in reverse order
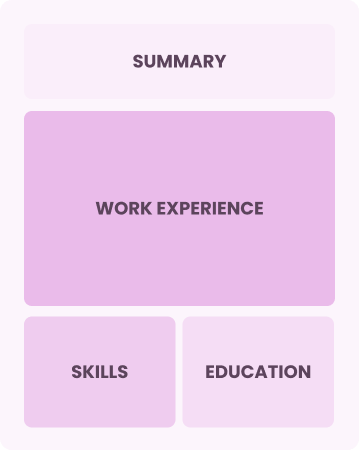
Best for:
Experts in strategic enrollment management and team leadership
Frequently Asked Questions
Should I include a cover letter with my enrollment specialist resume?
Absolutely. Including a cover letter can significantly improve your application by highlighting your unique qualifications and demonstrating enthusiasm for the position. It offers you a chance to elaborate on your resume and connect your experience directly to the job. For assistance, explore our comprehensive guide on how to write a cover letter or use our Cover Letter Generator for quick help.
Can I use a resume if I’m applying internationally, or do I need a CV?
When applying for jobs outside the U.S., use a CV instead of a resume. A CV provides a comprehensive overview of your academic and professional history, making it ideal for international applications. To ensure yours meets the necessary standards, explore our resources on CV examples and learn how to write a CV.
What soft skills are important for enrollment specialists?
For enrollment specialists, interpersonal skills like active listening, empathy, and communication are essential. They foster strong connections with potential students and colleagues, ensuring a seamless enrollment process and creating a welcoming atmosphere within educational institutions.
I’m transitioning from another field. How should I highlight my experience?
When applying for enrollment specialist positions, highlight your transferable skills such as customer service, organization, and communication. These abilities showcase your readiness to excel in this role, even if you lack direct experience. Use specific examples from your past work to illustrate how these skills can improve enrollment processes and improve client interactions.
How do I write a resume with no experience?
If you're looking to apply for an enrollment specialist position but lack formal work experience, don’t worry. Highlight relevant skills such as customer service, attention to detail, and any volunteer work or internships in your resume with no experience. Emphasize your ability to communicate effectively and your passion for helping others navigate their educational journeys. Employers value enthusiasm and a willingness to learn.
How do I add my resume to LinkedIn?
To increase your resume's visibility on LinkedIn, you can add your resume to LinkedIn by uploading it to your profile or highlighting essential skills and achievements in the "About" and "Experience" sections. This approach helps recruiters easily identify qualified enrollment specialists, improving your chances of being noticed by hiring managers in the field.